Helping physical therapy patients adhere to their exercise regimen
01
Responsibility
Designer, Prototyper, User Researcher
Timeline
April to August 2016
Team
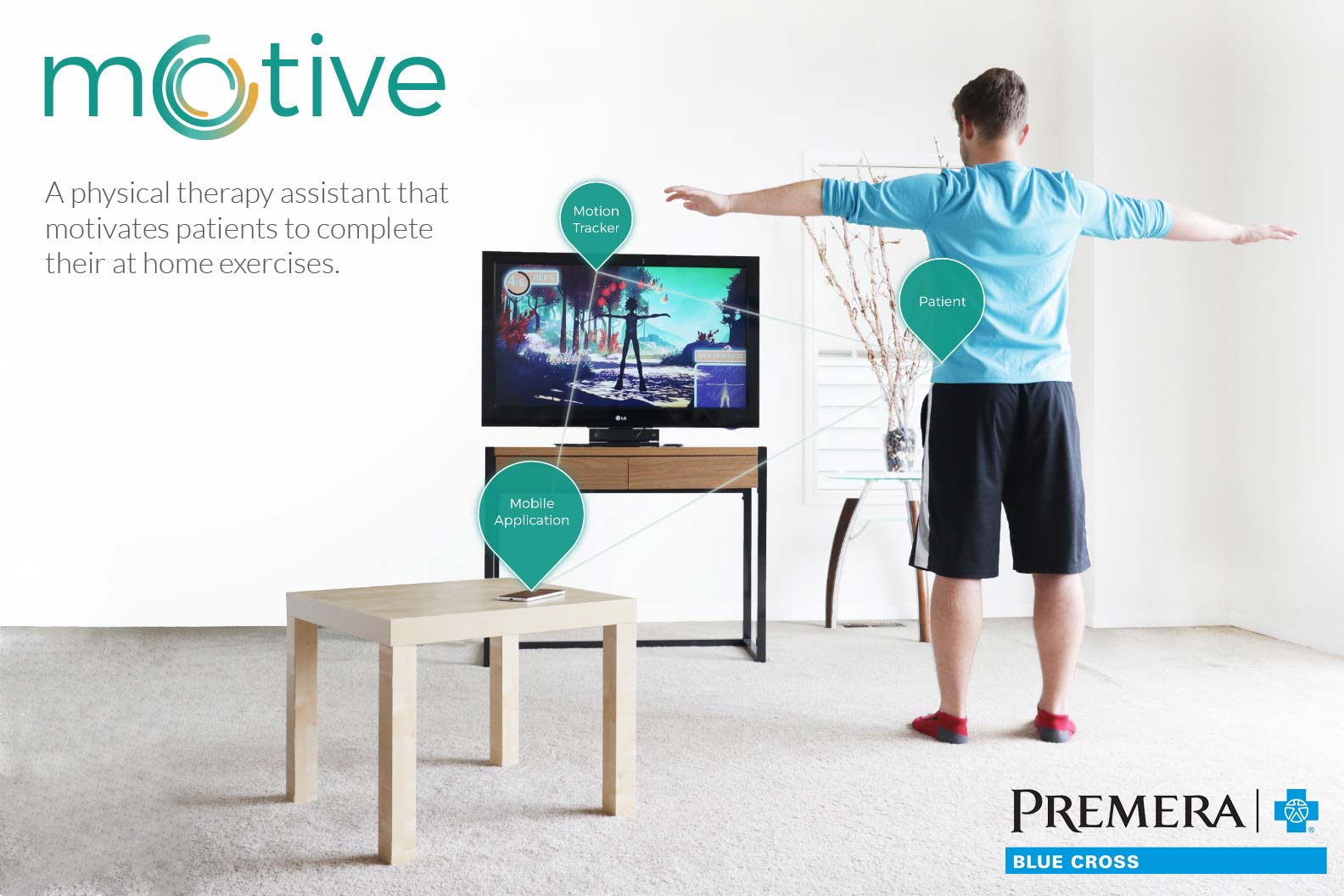
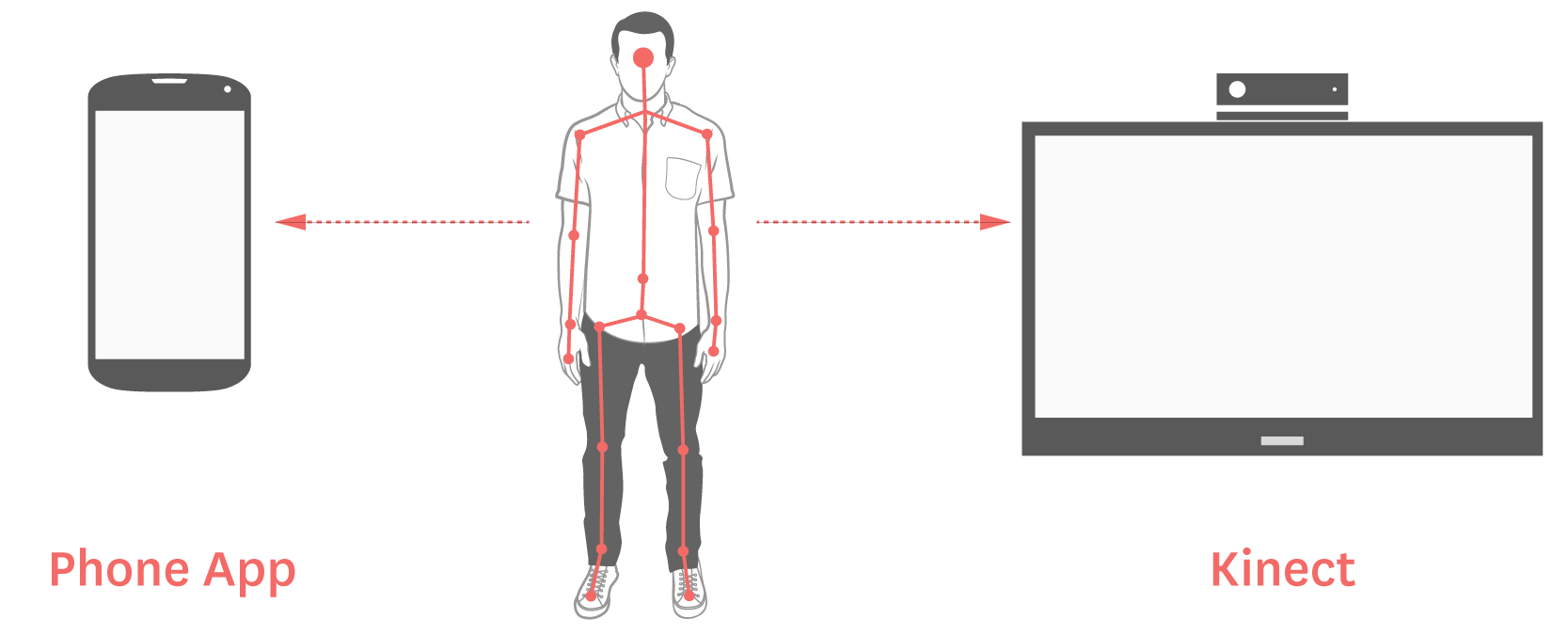
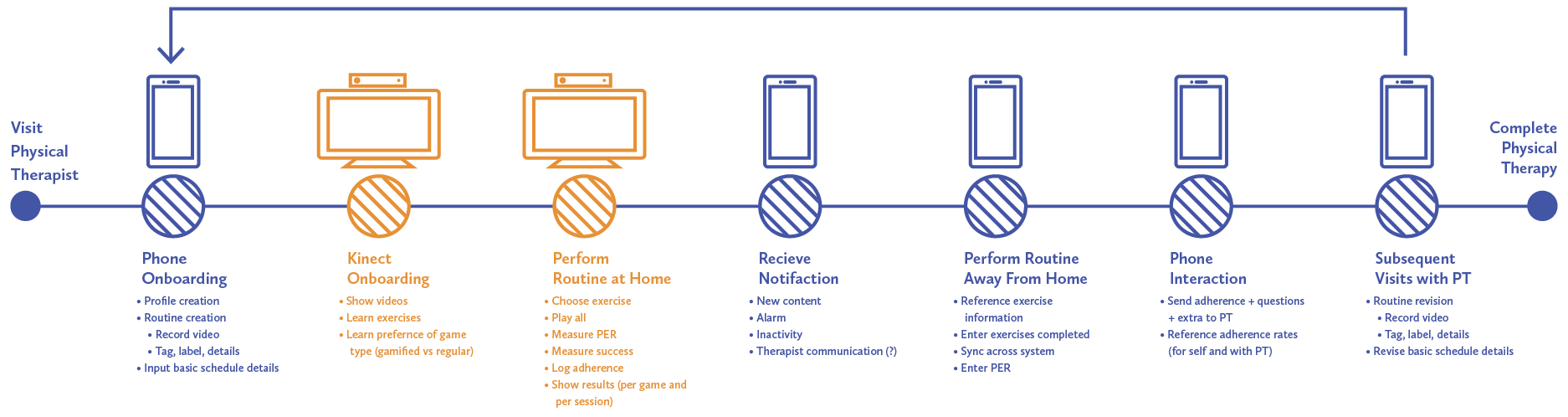
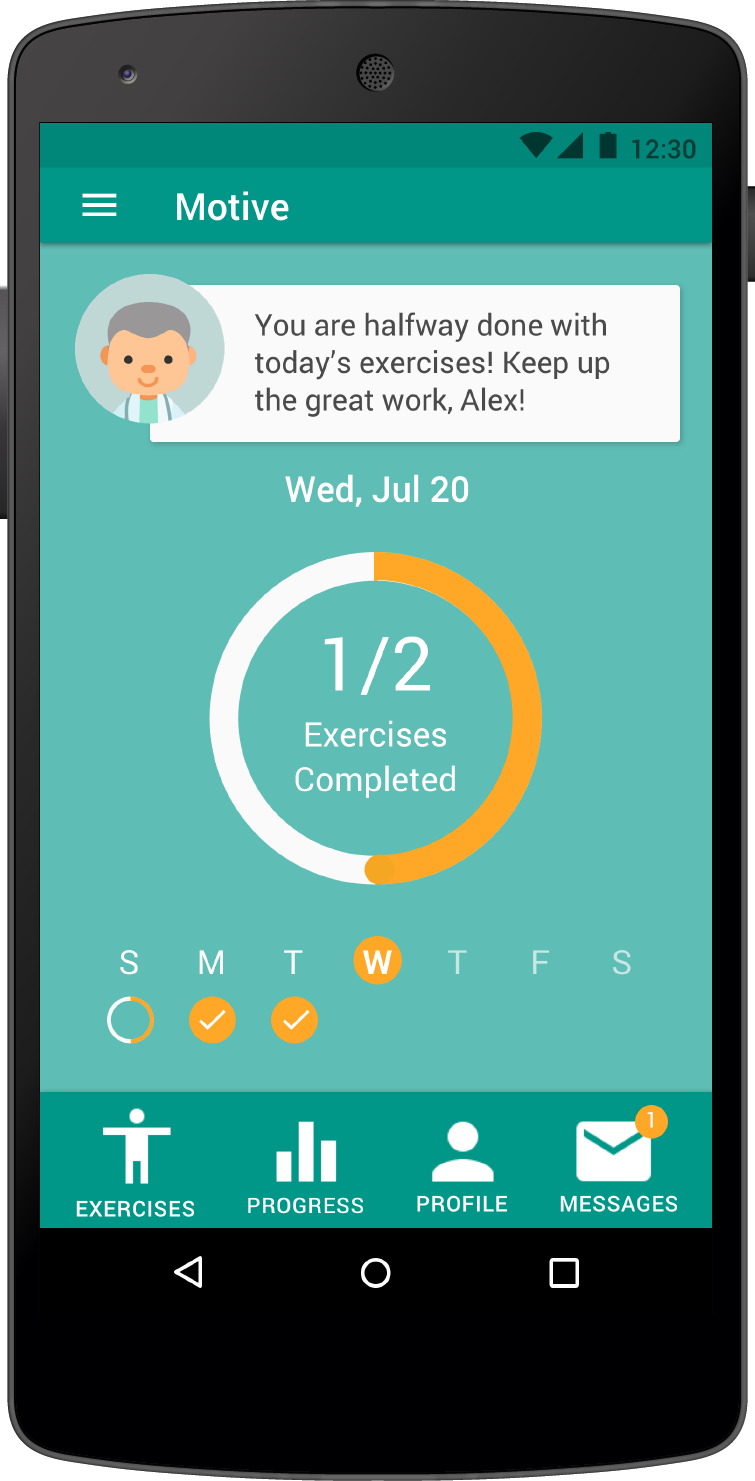
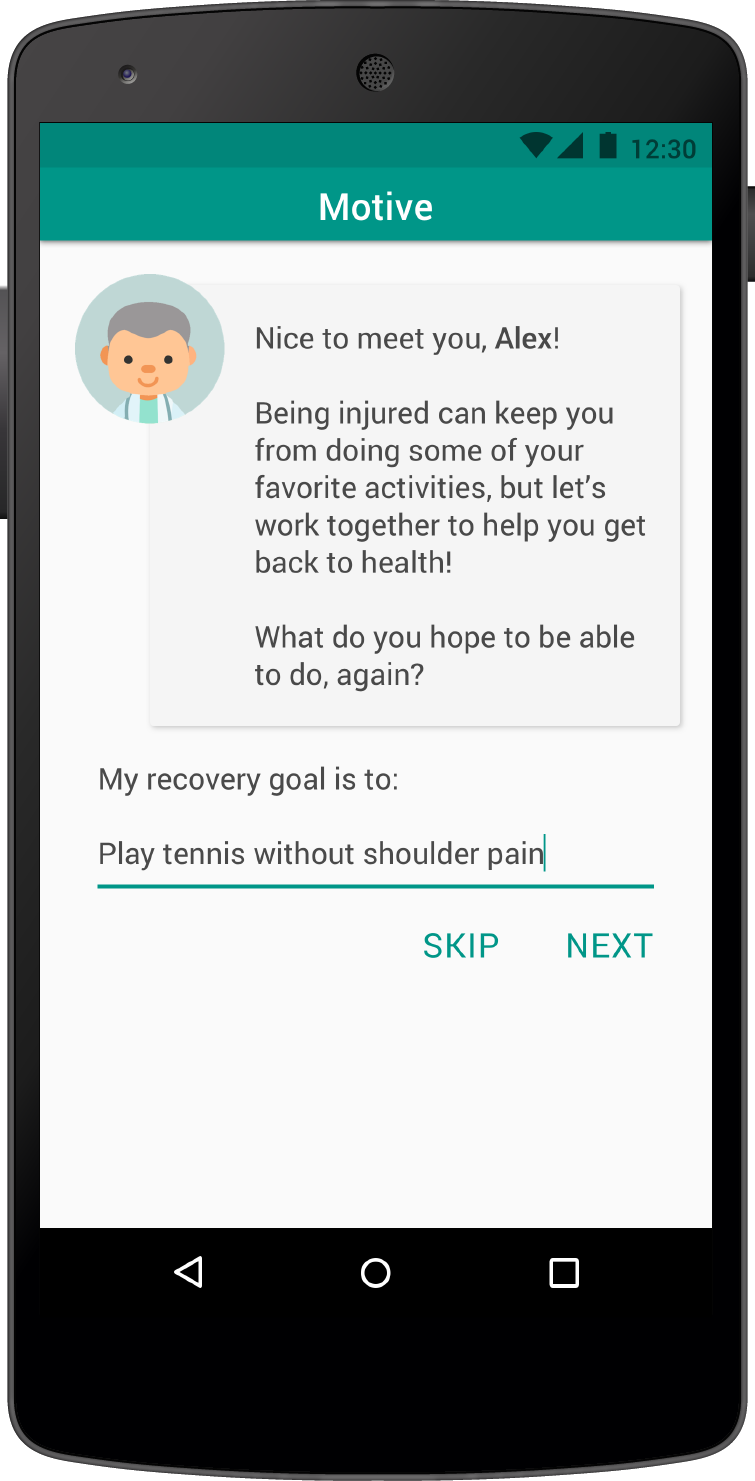
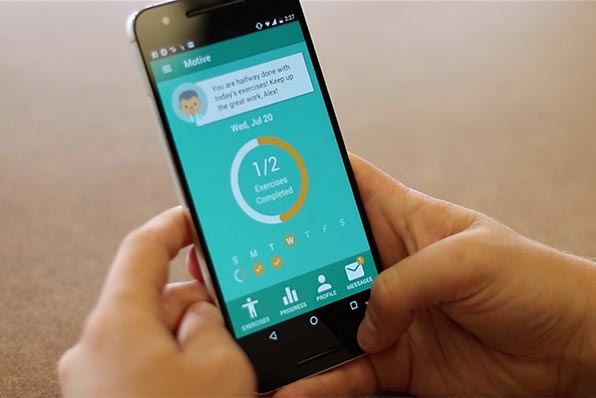
A physical therapy assistant that motivates patients to complete their home exercises through personalized reference videos, exercise reminders, engaging gameplay and thoughtful progress tracking. The Motive system consists of a standalone mobile app, which can be augmented with a home-based motion tracking.
Goal
How can we motivate adult physical therapy patients with acute, orthopedic injuries to adhere to their home exercise programs?
In the medical field, patient adherence is widely problematic. Physical therapy is no exception. Non-adherence with treatment and exercise performance could be as high as 70% ( Jack, Kirsten, et al).
Patients struggle to complete their home exercise programs. In turn, non-adherence slows a patient’s recovery, increases expenditures for medical care and may cause patients to doubt the value of the physical therapy practice as a whole. With this in mind, our team set to work empowering patients to take control of their recovery and get back on track. We framed our exploration using the following design question
Secondary Research
To better frame our project, we began with secondary research in the form of a literature review, competitive analysis and popular media scan. We learned that current tools for physical therapy adherence are not working because
-
Current Tools try To Replace The Role Of The Physical Therapist
A physical therapist’s ability to assess pain in context is imperative to creating a successful treatment plan (i.e. augment, don’t replace).
-
Current Tools DO NOT ACCURATELY REPRESENT THE PATIENT’S EXERCISES
Paper reference sheets use stock images or hand drawn figures to convey movement. Patients quickly forget what they mean.
-
Current Tools ARE NOT PERSONALIZED TO A PATIENT’S NEEDS
Physical therapy exercises are highly customized based on the ability of the patient. Many systems do not adapt to these changes.
Primary Research
Our primary research was framed by our secondary research and offered rich, first hand accounts of stories and experiences. Below are a few interesting snapshots which helped us understanding the problem space:




-
Subject Matter Expert Interviews × 7
- We interviewed 7 physical therapist with different specializations to learn about tools, methods, and tricks typically used by them.
- Learned about the kind of information physical therapists needed to successfully support their patients.
-
PATIENT INTERVIEWS × 6
- We interviewed 6 patients spanning different self-identified adherence levels, and stages of treatment.
- Learned about challenges beyond adherence. Eg: Patient are not aware doctors want to know day to day details of their lives.
-
EMPATHY BUILDING EXERCISES × 2
- We went through the experience of visiting a doctor from Patient's POV.
- We were assigned home exercise routine by the doctor which helped us to understand challenges faced to complete them.
-
CONTEXTUAL INQUIRIES × 4
- Observed current patients home exercise routines in the locations that they typically completed them.
- We observed environmental factors that may have affected their adherence.
Research Synthesis
Identifying opportunities
At several points along the way, the team discussed our findings and used affinity mapping, interview coding, concept diagrams and discussion to evaluate our results. Below are journey maps and design principles.
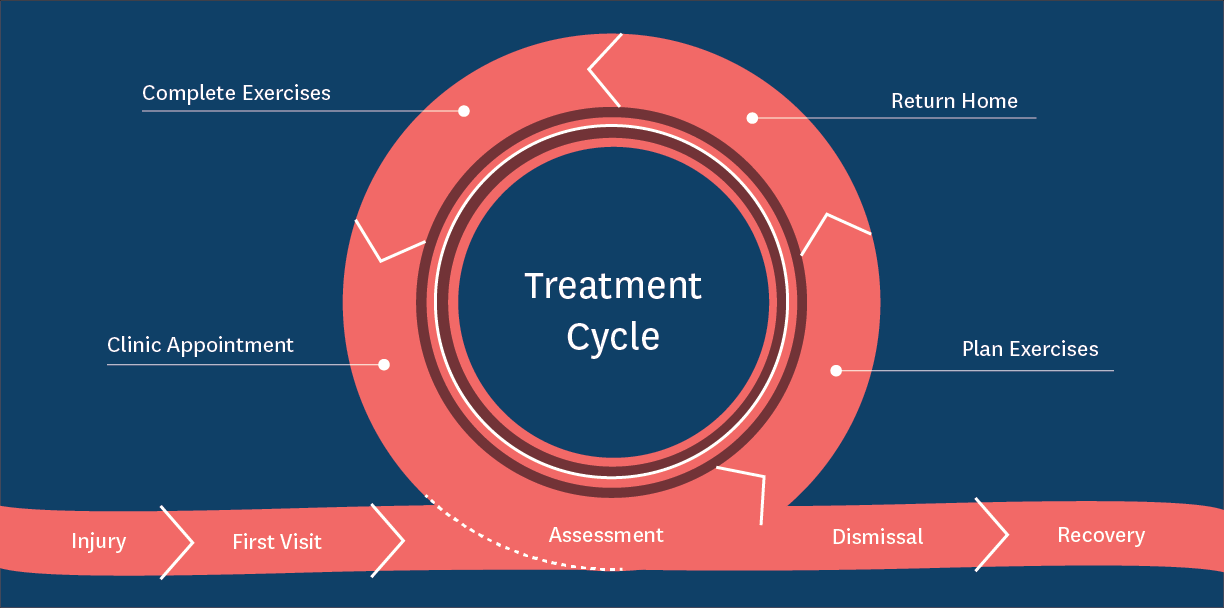
Ideal Experience
Prior to our primary research, we were under the impression that the patient experience looked like the first diagram.
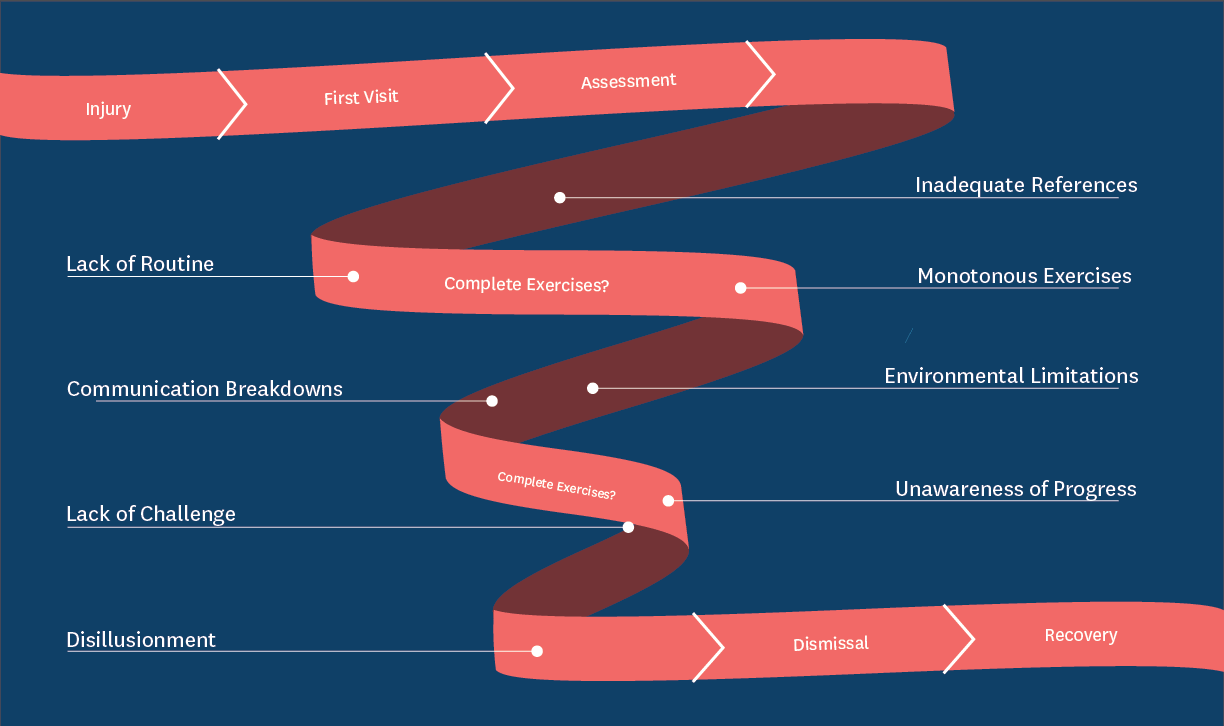
Current Experience
However if we pull apart the treatment phase, we see instead of being a consistent loop, little breakdowns along the way start to compromise a patient’s path to recovery.
Design Principles
After analyzing our qualitative data, these findings were later incorporated into a set of design principles, which drove the ideation phase of our project.




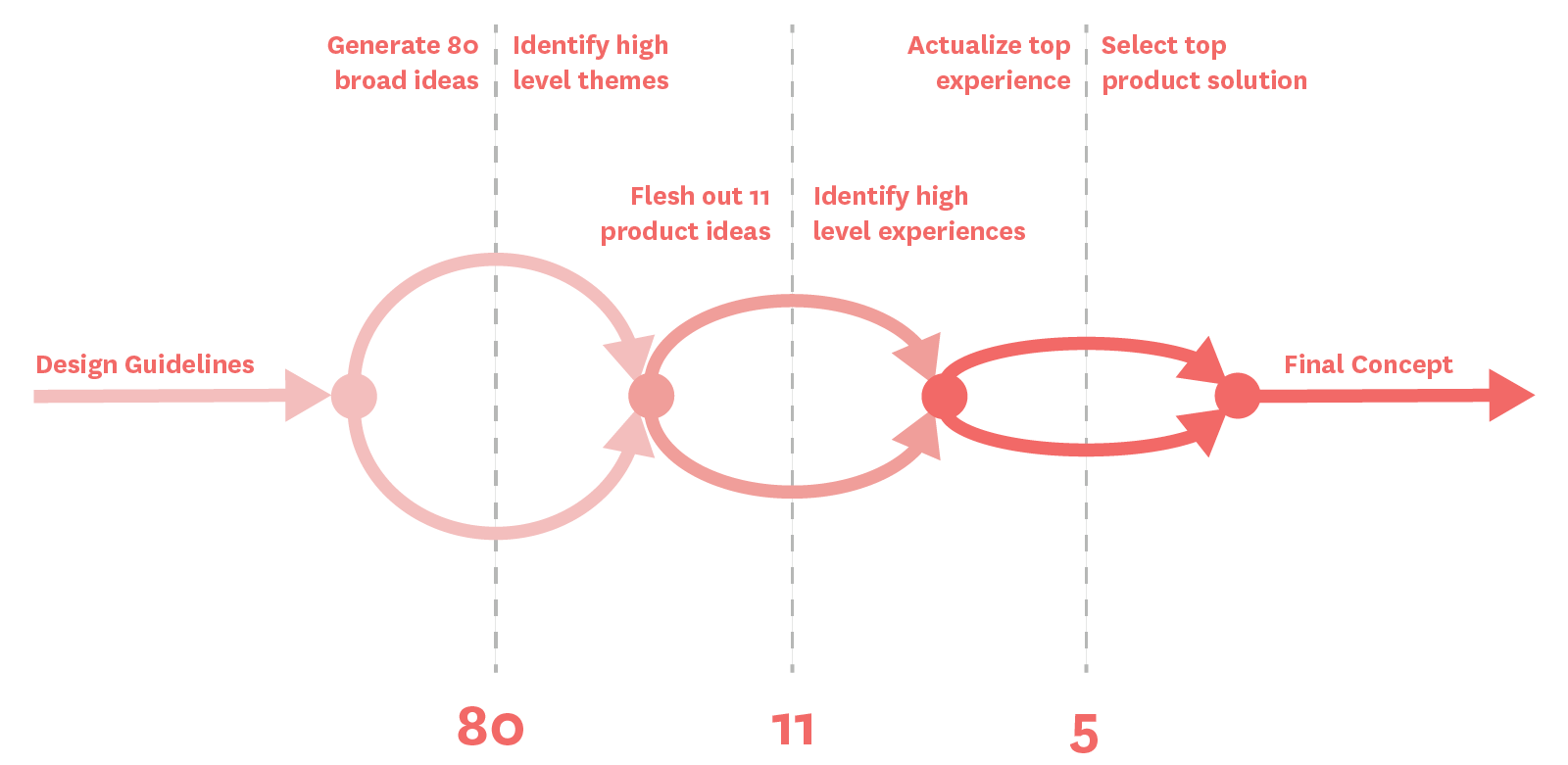
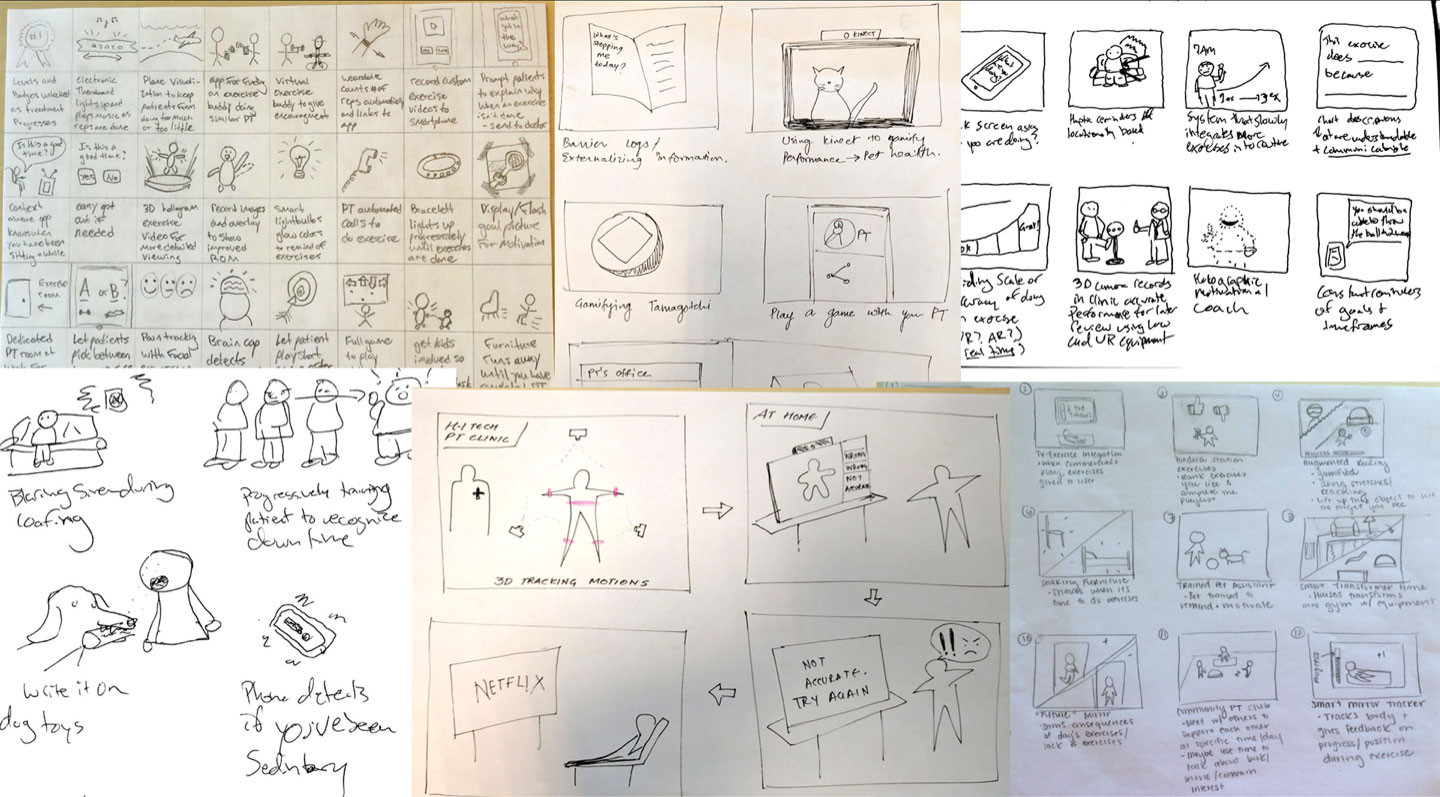
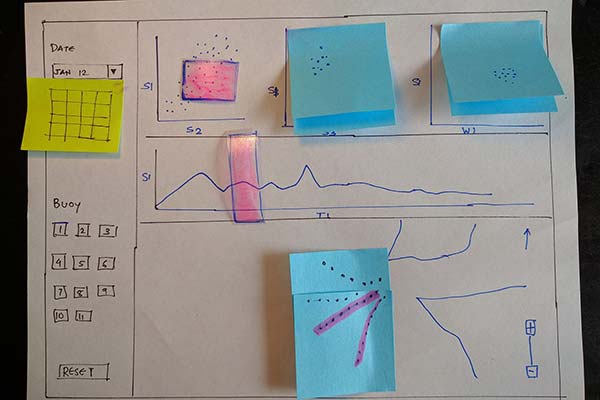
Ideation
Our team spent 2 weeks avidly brainstorming, sketching and storyboarding potential design solutions from improved paper exercise sheets to virtual reality clinics. We were able to narrow down our 80+ ideas by continuously categorizing concepts, identifying overarching themes or principles, and using them to refocus our explorations.
Broad Ideation
We began our ideation by creating a set of prompts, drawn from our user research. These prompts were used as inspiration during sketching exercises and to make sure we addressed the full range of pain points in the physical therapy experience.
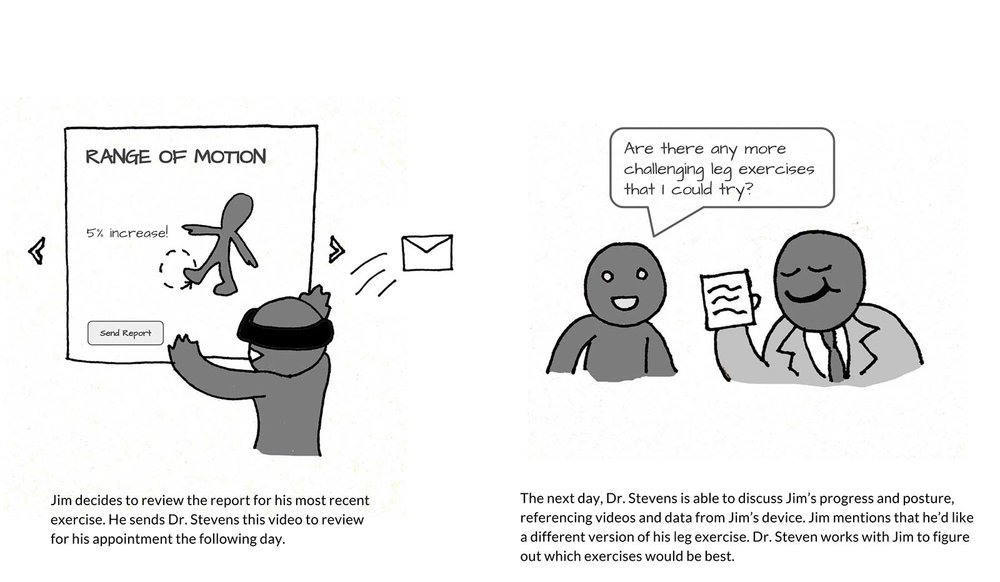
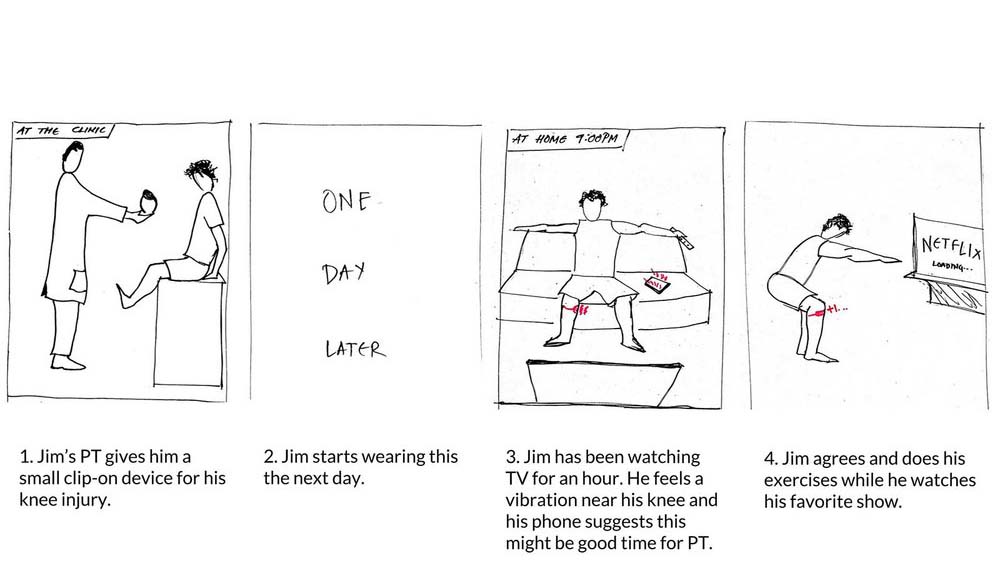
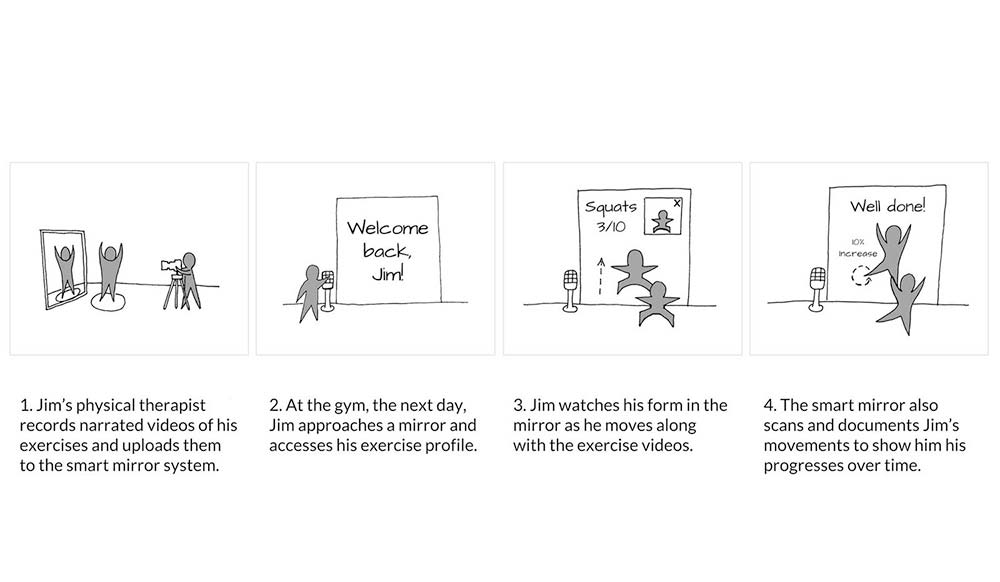
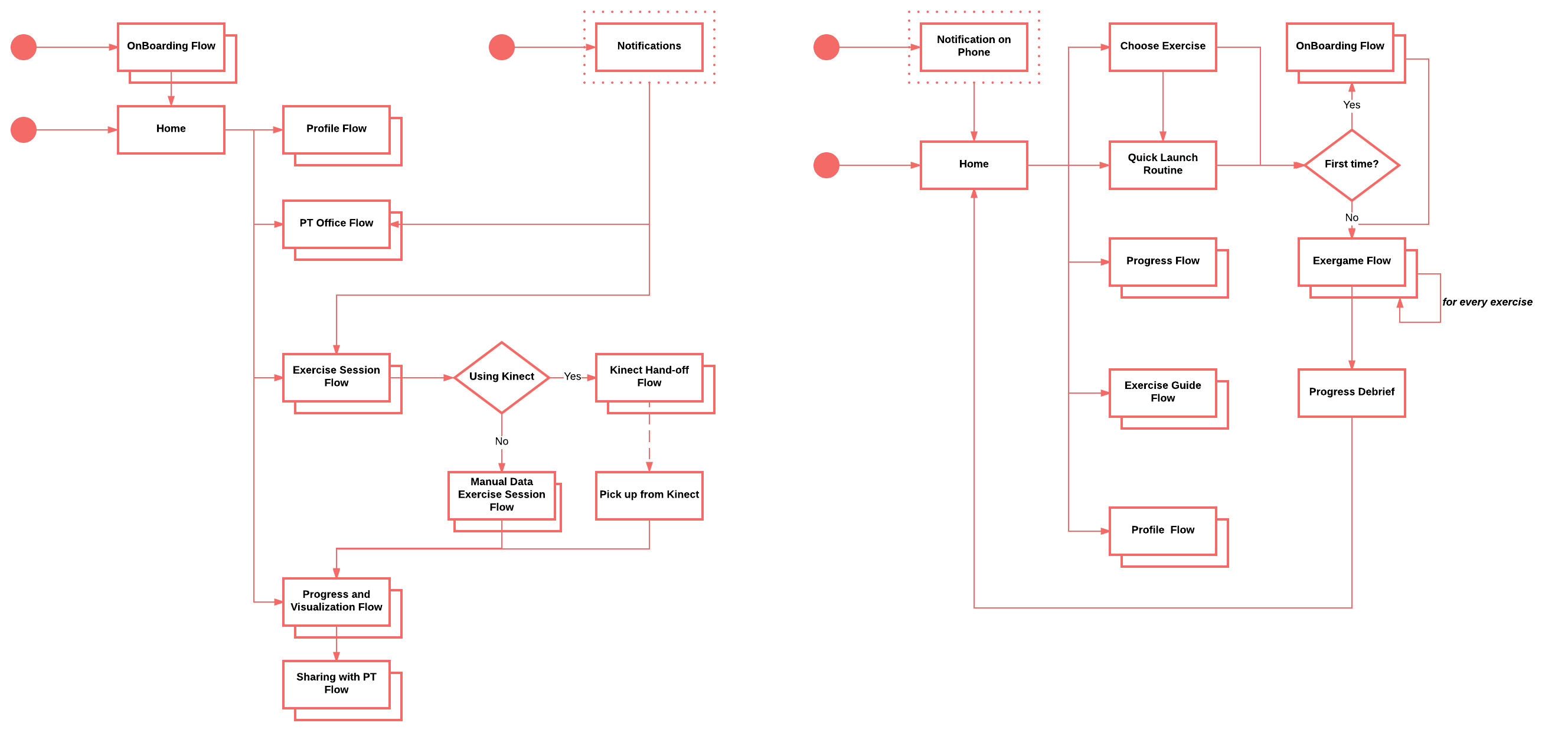
Imagining the experience
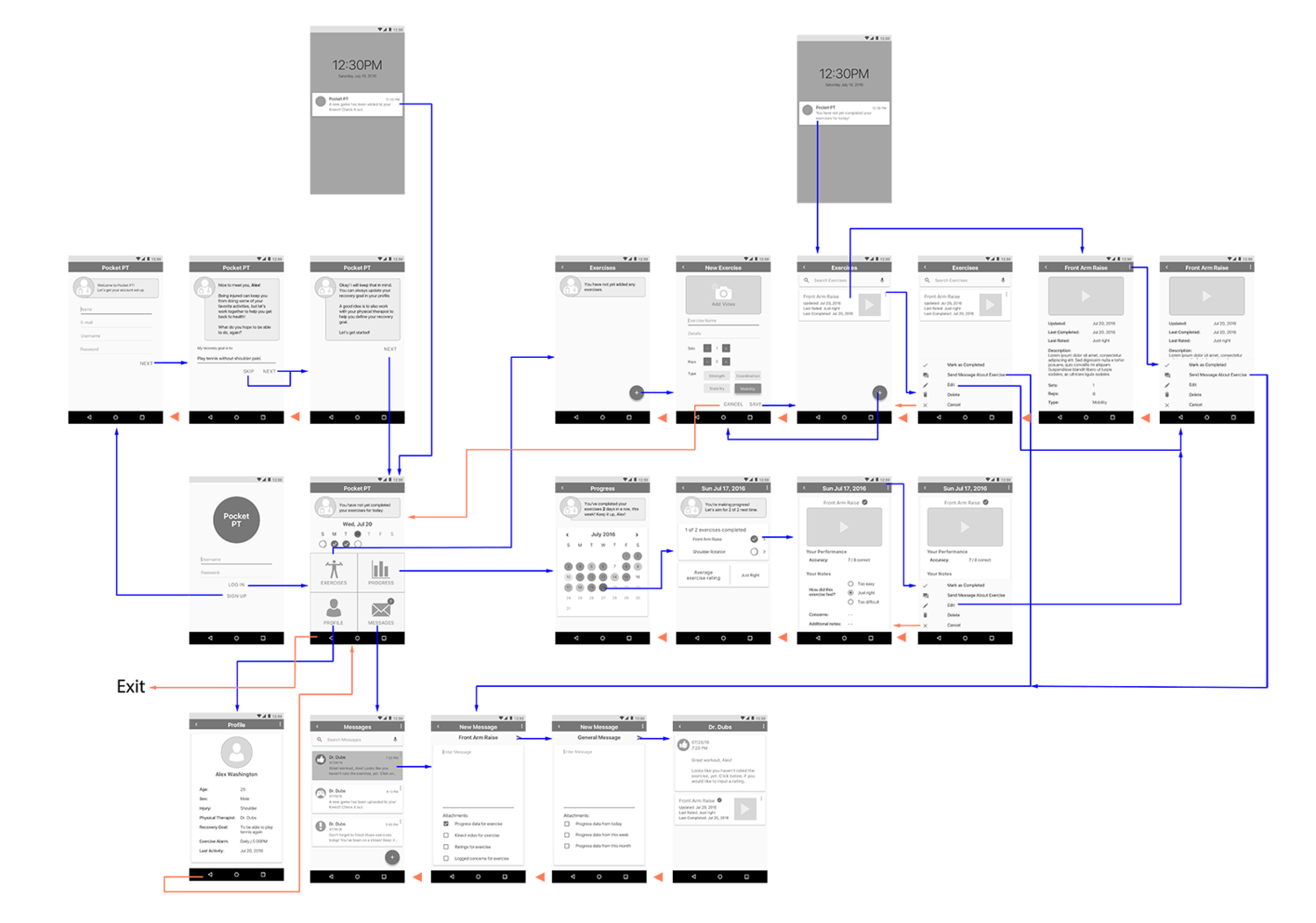
Before creating high-fidelity prototypes, I made wireframes and tested them with instructors to find common usability issues with the new interaction style.
Final Direction
In our process, we created a list of values that reflected qualities the solution should have. We vetted solutions we had against these values and arrived at our final product, Motive.
MAPPING TOUCHPOINTS, FEATURES TO EXPERIENCES
Prototyping
Testing early, often and cheaply
In the end, we made high fidelity and functional prototypes. However, to reach that point we relied heavily on cheap and fast techniques like sketching, power point, Wizard of Oz testing and InVision to test our ideas.
Phone App Sketches
We started sketching app screens with focus on information architecture
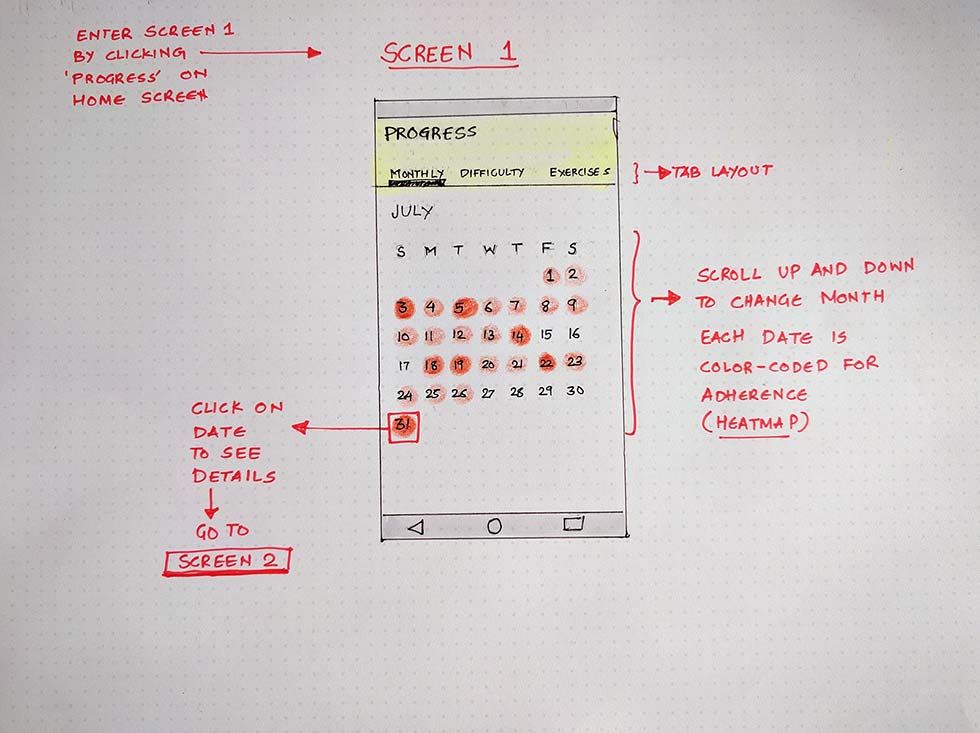
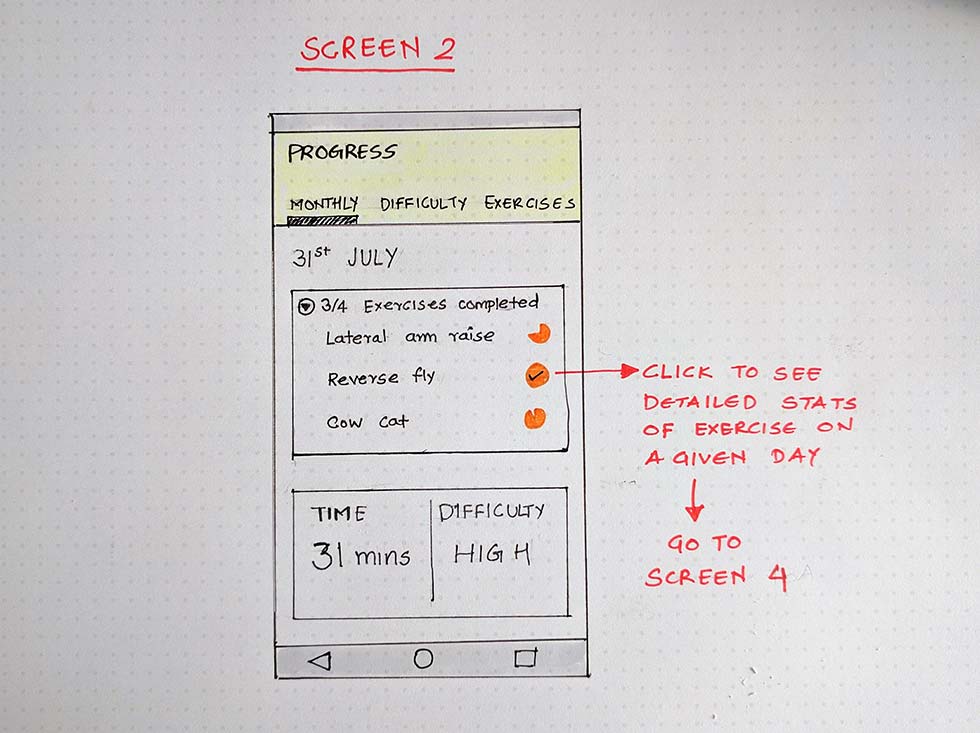
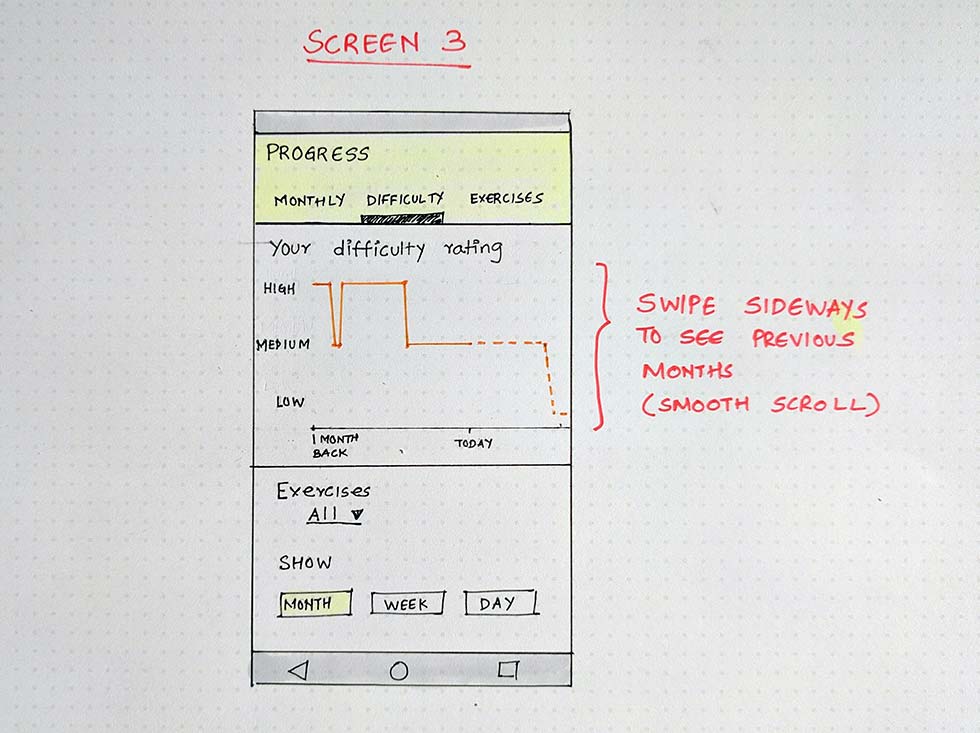
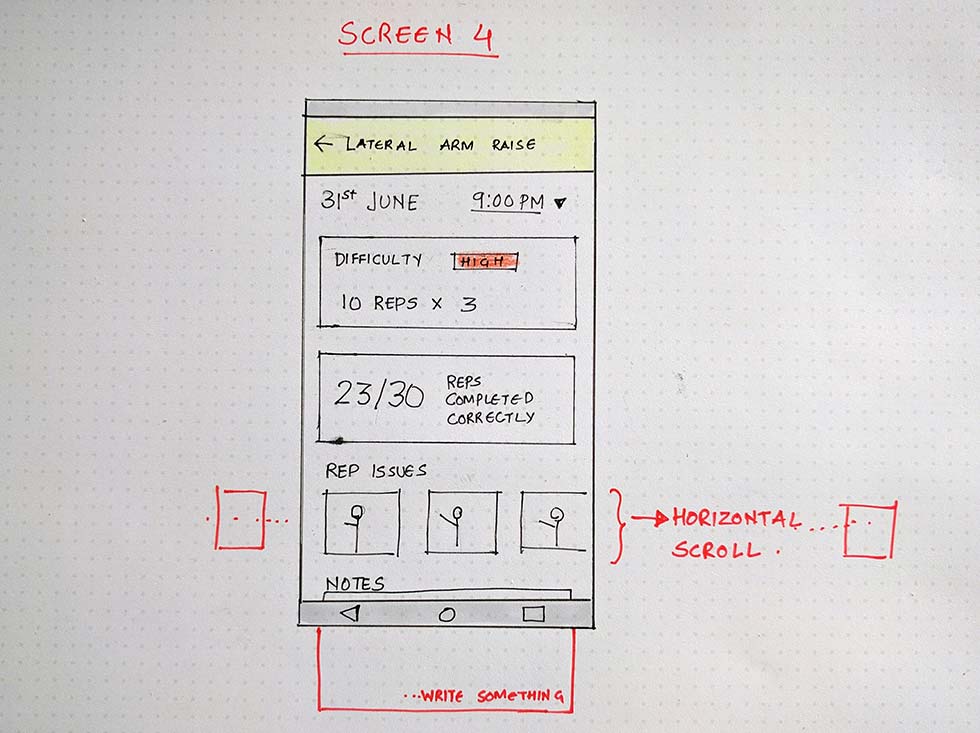
Wireframes
Once we had tested our first round of phone app sketches with patients and physical therapist, we decided to start making wireframes to further test our design.
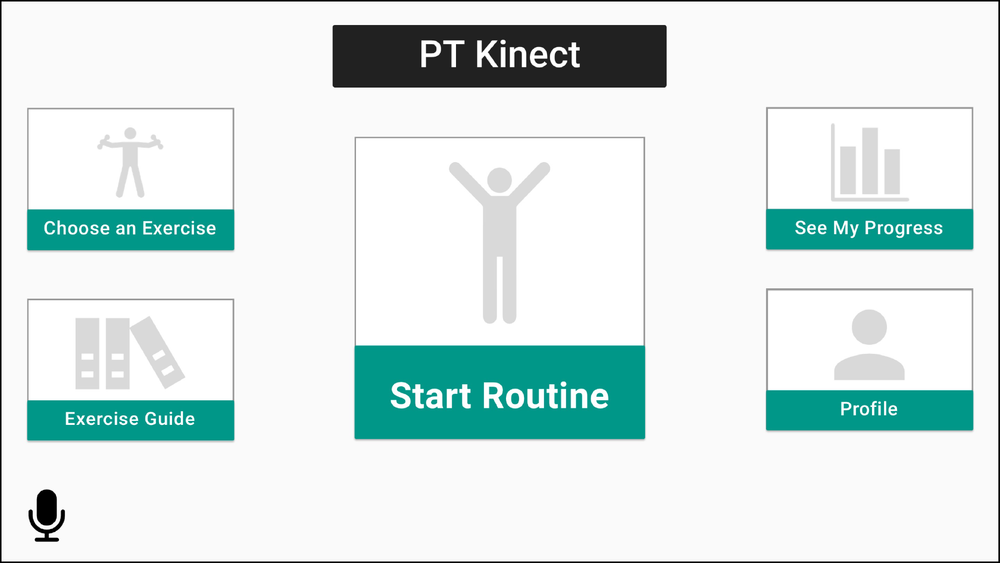
Kinect Prototypes
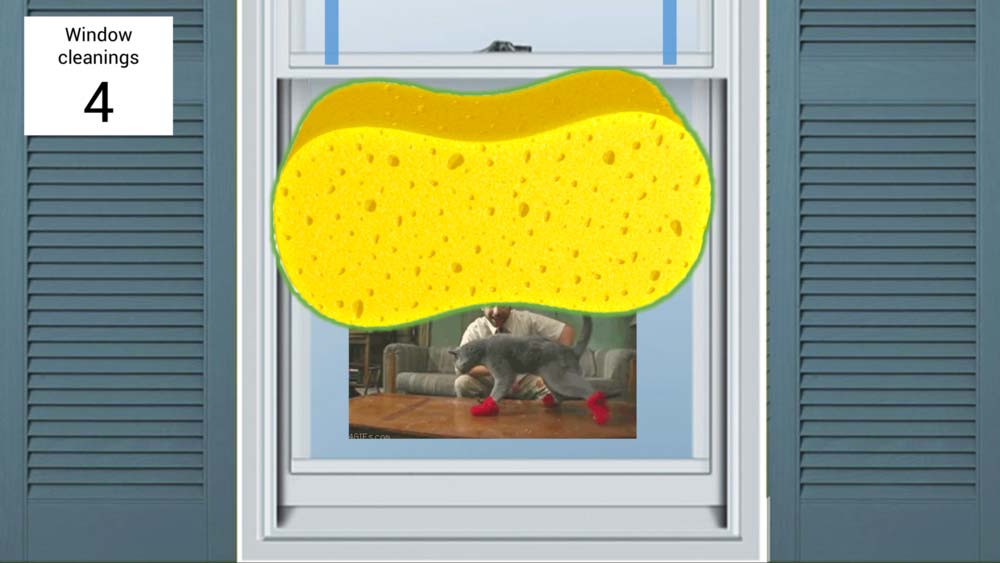
The Kinect prototype relied on a mix of Wizard of Oz style PowerPoint animations and video overlays.

Evaluation

Design Hypothesis
Through our prototypes, we wanted wanted to test usability and assess whether our designs added value. Our design hypotheses were as follows:
-
Exercise References
Narrated video references will increase a patient’s confidence when completing exercises at home.
-
Engagement
Gamified exercise experiences will keep patients more adherent than unprompted physical therapy.
-
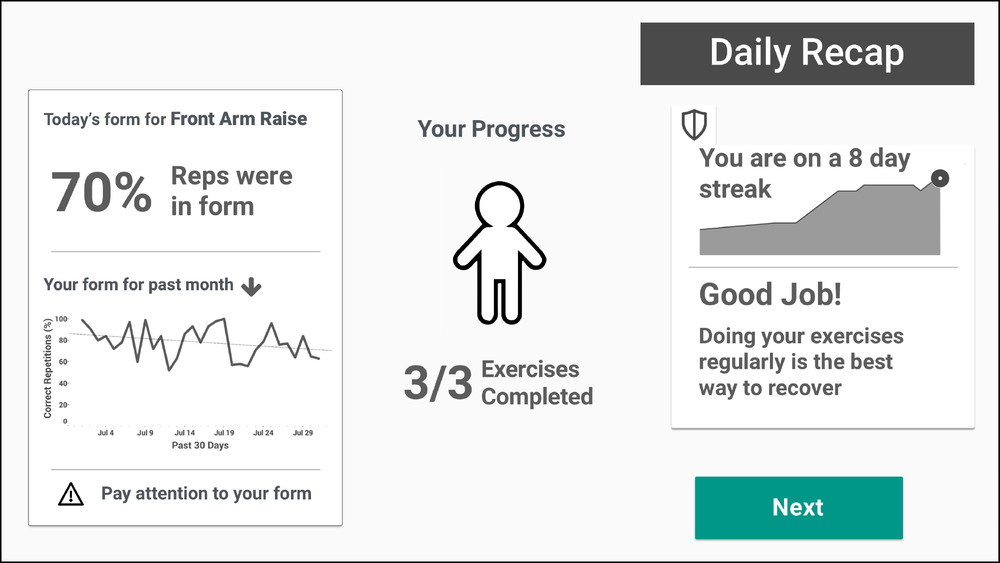
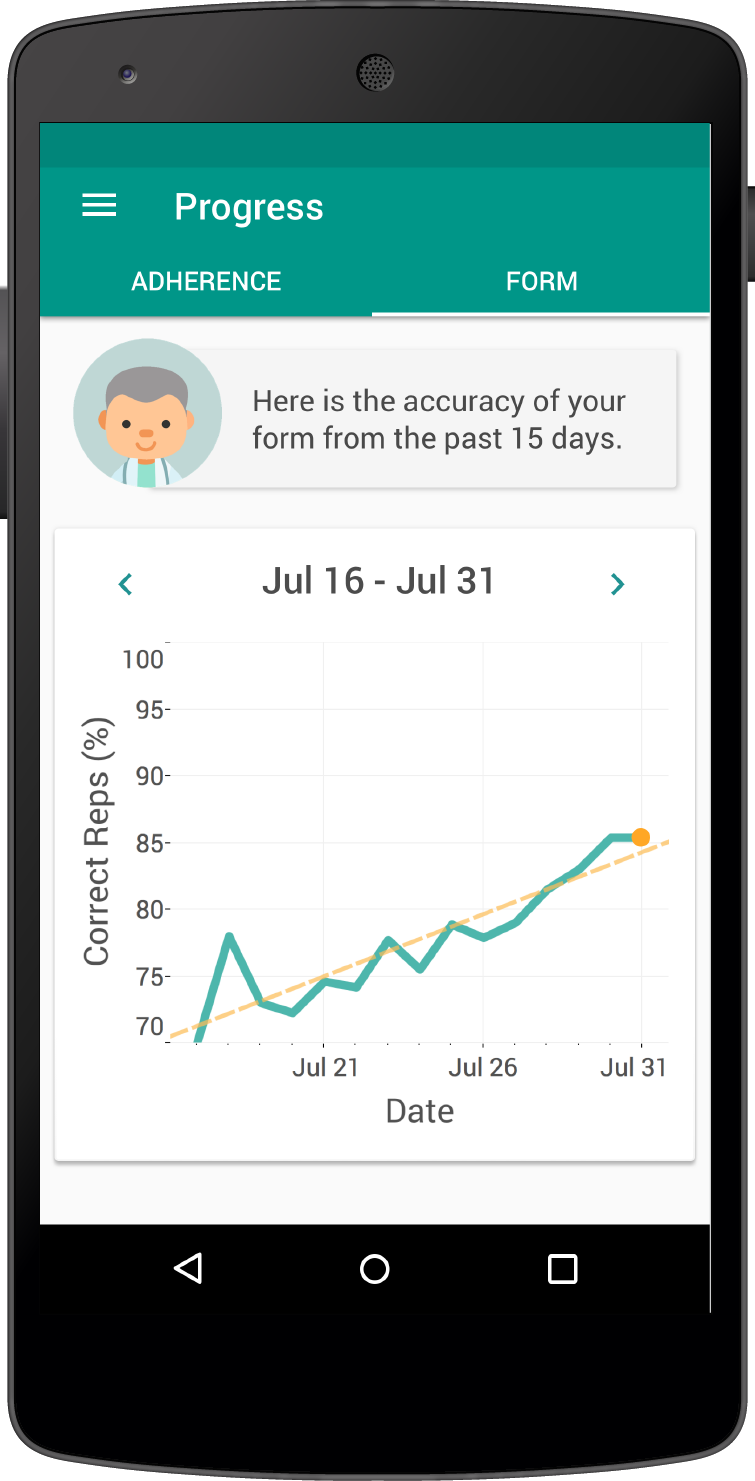
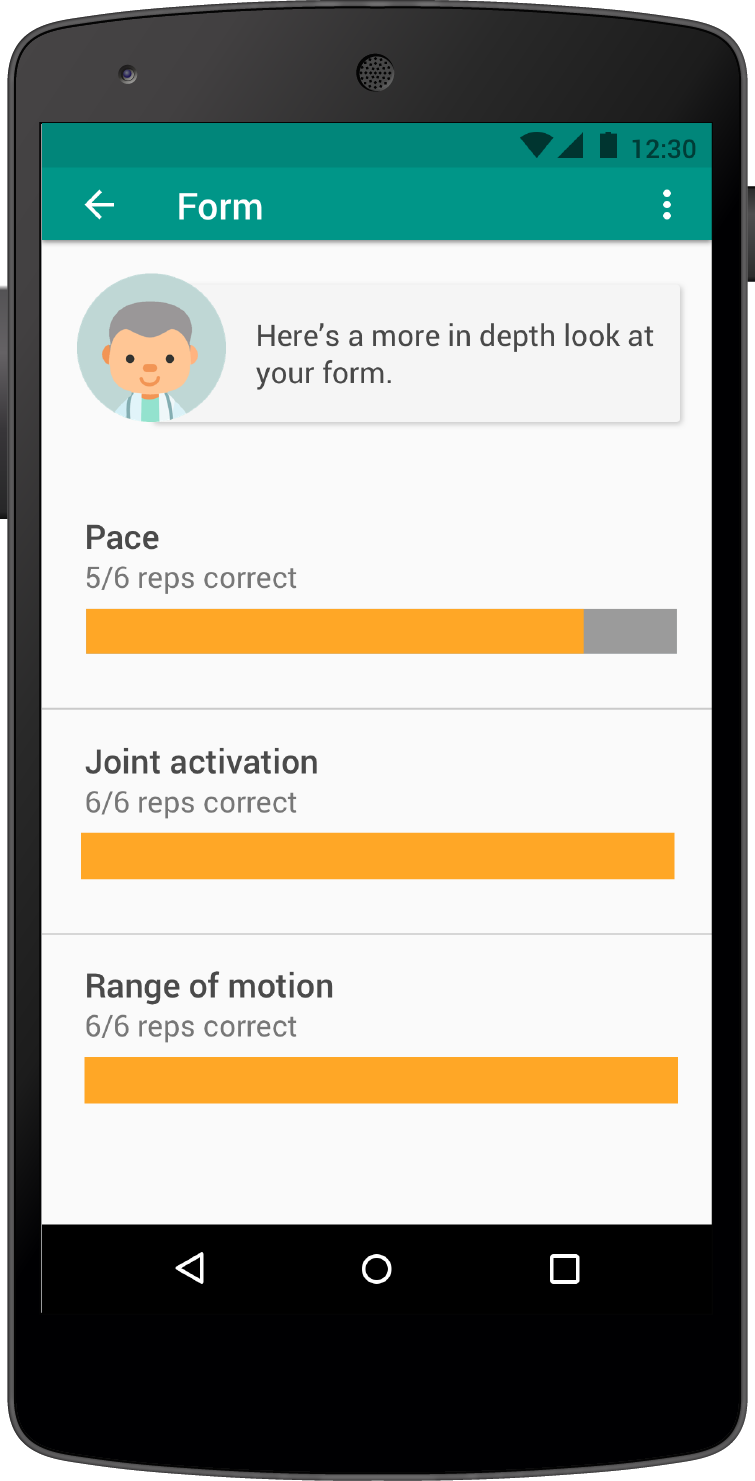
Progress & Motivation
Explicit progress tracking will motivate patients to adhere to their prescribed exercise regimens.
Behavioural Prototypes
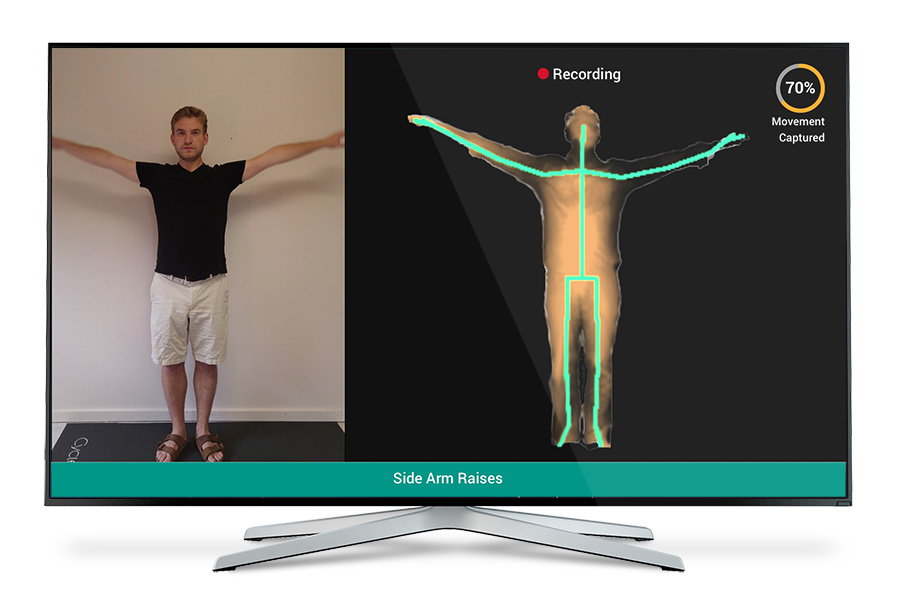
We used rapid prototyping techniques to maximize feedback, using minimal resources. The Kinect prototype relied on a mix of Wizard of Oz style PowerPoint animations and video overlays. To add context, all of these components were incorporated into a behavioral prototype, during which participant’s were taught an exercise and walked through a mock physical therapy scenario.

Feedback
We tested our prototypes with six recent and current orthopedic physical therapy patients before reaching saturation. Through the use of structured scales, we found that Motive improved participants’ confidence and likelihood of completing exercises.
-
Video Recording
Video recording continues to be a cornerstone of our value proposition and user experience.
[The video] basically removes all doubt.
— Participant 2 -
Real Time Feedback
In gameplay, users must either be able to see their movements or be given feedback on form.
I still don’t know if I’m doing it correctly in real time.
— Participant 1 -
Game Distraction
Certain game elements were distracting. Moving forward, games should presents the player’s real-time movements as a focal point, while subtle yet interesting animations unfolded around it.
I completely forgot to focus on my shoulder blades because I was completely distracted by wondering what I was going to see next.
— Participant 4 -
Progress Visualization
The adherence streak’s ambiguous graph was confusing. But overall progress visualizations instilled patient confidence in their recovery
I could imagine the app being a great option for when I’m traveling and don’t have a Kinect on hand.
— Participant 2 -
Companion App
Participants reported that they found the mobile companion application very useful, even without the Kinect.
It’s in a visual form, so [the progress visualization] tells me I’m making progress even if I don’t know if I am.
— Participant 2
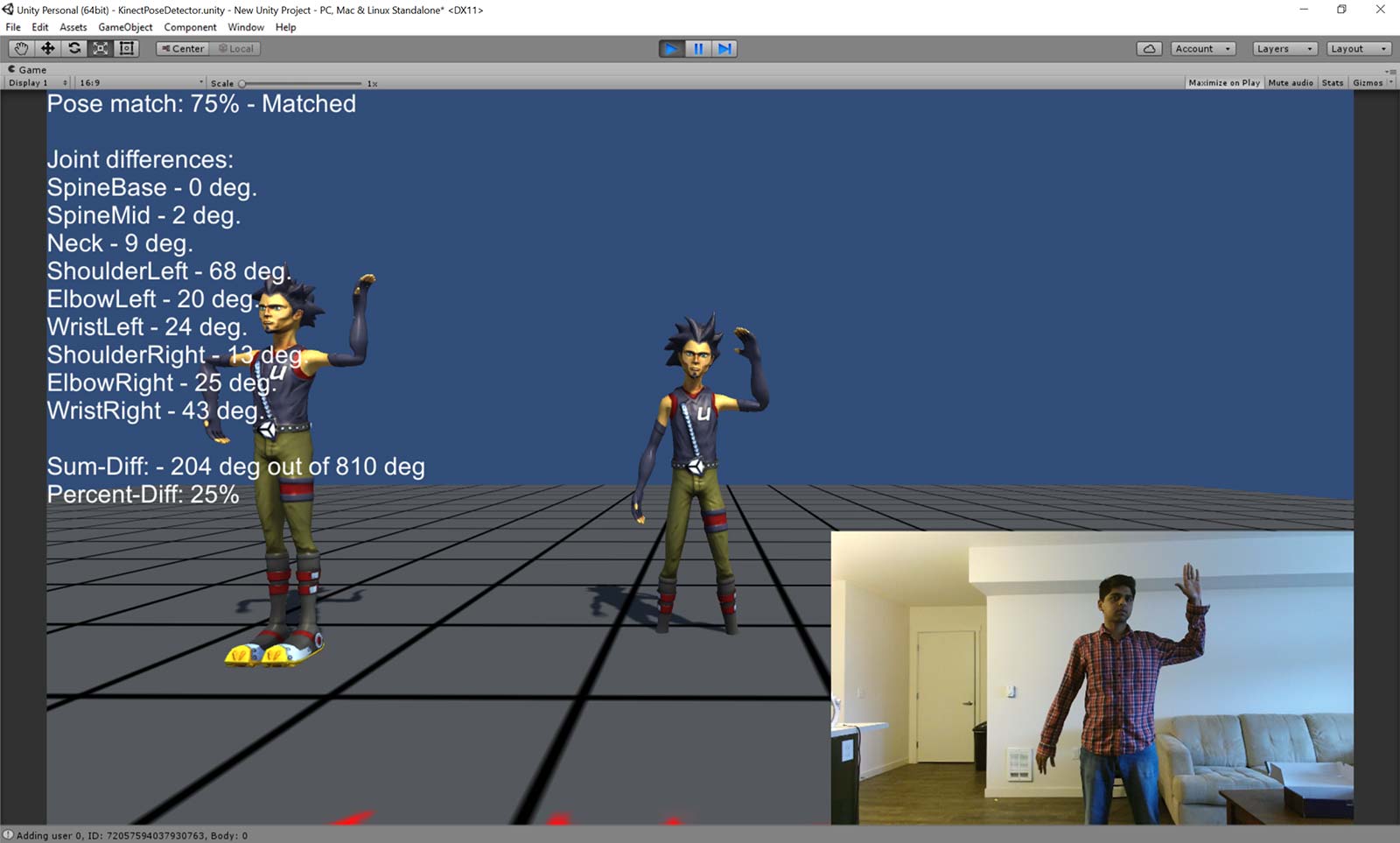
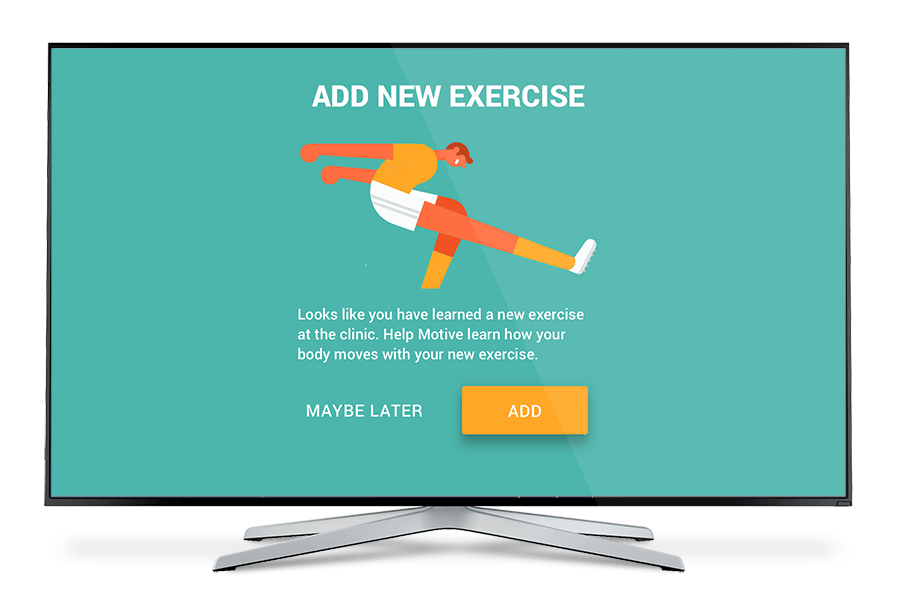
Proof of concept
I built a feasibility prototype in Unity to quickly validate the degree of accuracy we can achieve. This would later help us in designing the feedback and progress capture. I tested accuracy, edge-cases and reliability of motion tracking in different environmental and exercise scenarios. Kinect was reliable and accurate enough for most of our test cases. Kinect provided the right resolution of accuracy to provide meaningful feedback based on relative joint movement and angle.
Fine tuning
Here I am fine tuning different variability in accuracy of different joint movements.
Outcomes
Functional Prototypes
Based on user feedback, we revised our designs and created high-fidelity prototypes of our product. A functional Kinect Prototype was buit in Unity 3D and we made one game which worked with Kinect to measure accuracy of side arm raises.


Reflection
Moving forward, we would like to dive deeper into game creation, in collaboration with physical therapists and experienced game designers. Next, we would like to expand this system to a broader demographic of patients. After reaching HIPAA compliance, we also see Motive being extended to better serve the needs of physical therapists. A highly usable provider portal would keep patient information organized and easily accessible for clinicians.
Other Projects
product
01
Helping physical therapy patients adhere to their exercise regimen
view solution
web-app
02
Helping instructors deliver better eLearning experience
view solution
Visualization Standards
03
Helping oceanographers build visualization standards
view solution
Physical Computing
04

An intelligent device to monitor healthy backpack use
view solution
Prototyping
05